|
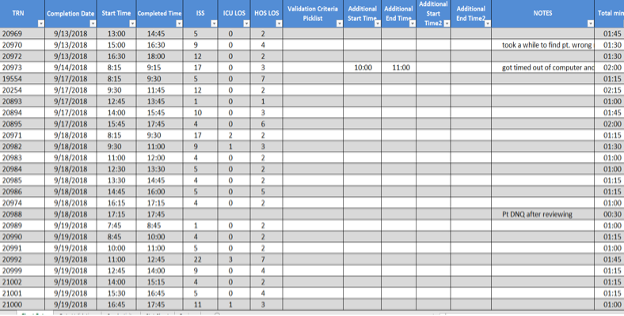
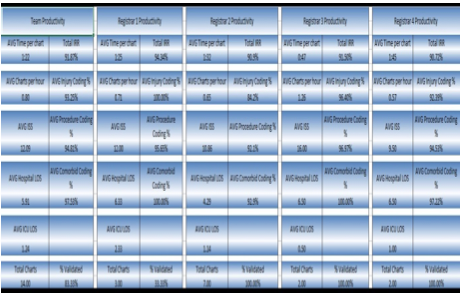
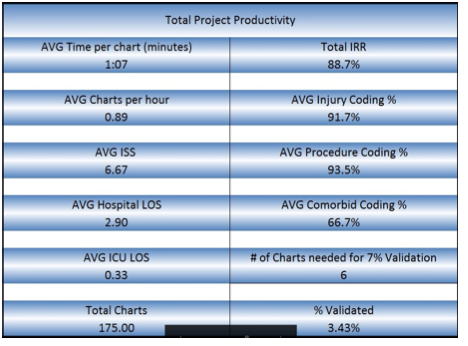
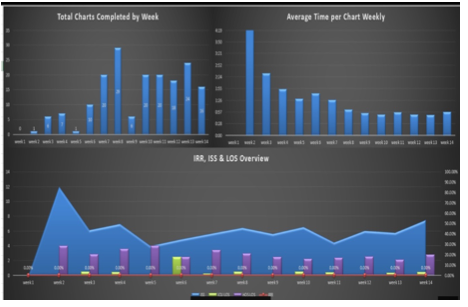
Manpower is a common term we use in every industry. In healthcare, it takes on a slightly different level of importance. Here, we try and balance job responsibilities and expectations with budgets and deadlines. There is no better example of this tight rope act than with the trauma registry. The “manpower” of the trauma registry staff is unique. They are to identify patients, abstract all the data that is needed, enter it into the trauma registry, perform data validation, run reports, and submit all this error free data to the state and national trauma registries on a quarterly basis at a minimum of 80% compliance rate. This of course takes a lot of “muscle power” to complete this daunting task. Therefore, the age-old question remains, how many charts should my trauma registrar complete in a day, week, or month. This is a multi-layered question at best. Let us first review the full-time equivalent (FTE) employee statement from the American College of Surgeons (ACS). In Chapter 15 of the Resources for Optimal Care of the Injured Patient 2014 book, they list staffing as a criteria deficiency. “The amount of time and effort that will be necessary to maintain the registry should not be underestimated. A designated and well-trained trauma registrar is critical to the success of a registry. One full-time equivalent employee dedicated to the registry must be available to process the data capturing the NTDS data set for each 500-750 admitted patients annually (CD 15-9)”[i] This is a powerful statement, and one that is widely mis-used, or underestimated. As we begin to look at the statement the first element to focus on is the importance, they place on the trauma registry and its well-trained trauma registrar. They even go as far as to state the trauma registrar is critical to the success of the registry. The next key point is the FTE number “for each 500-750 admitted patients annually”. This is the first decision point to consider. Admitted patients annually. According to the National Trauma Data Standards (NTDS) Data Dictionary for 2021 “admitted” is listed as: “patients directly admitted to your hospital (exclude patients with isolated injuries admitted for elective and / or planned surgical interventions, OR patients who were an in-patient admission and / or observed.”[ii] With this clarification, elective or pre-planed surgery patients are excluded as well as emergency department (ED) discharges (unless they were admitted and boarded in the ED or stayed in the ED for observation). This is a rather pivotal statement. Some hospitals make the decision to capture or include all trauma activations in their trauma registry whether an admission or an ED discharge. This is an increased workload which is not included in the 500-750 FTE recommendation. Therefore, if your hospital does this, or is required to submit this data to your state trauma registry, your FTE per admission will be slightly different. The next pivotal part of the CD 15-9 language is the notation of the data captured. In the ACS language they clearly state “one FTE dedicated to the registry must be available to process the data capturing the NTDS data set…” This portion of the criteria deficiency is most often omitted. What does this truly mean? The NTDS data set are the data elements listed in the NTDS Data Dictionary. For 2021 all hospitals are required to report the 116 NTDS data elements, and Trauma Quality Improvement Program (TQIP) centers report and additional 31 data elements and there is 1 optional element for the national provider identifier (NPI).[iii] Therefore, a TQIP center that reports the NPI is reporting 148 data elements. Be advised that injuries and procedures are only one unique data field but will have multiple entries. Review the NTDS data elements, and you will not find data fields such as but not limited to personal health information (PHI) such as patient’s name, street address, medical record number (MRN) or account number. In 2021 the EMS patient care report universally unique identifier (UUID) number was added, and the majority of the prehospital data was retired. This, however, does not mean that the state trauma registry, nor your internal performance improvement (PI) program no longer requires this data. Therefore, it may still be in your trauma registry. Hospital level trauma registries capture a wide range of data elements needed for their internal PI programs. Data such as but not limited to transfer hospital details, vital signs, and procedures, or specific labs or drug administration. They may also require data on SBIRT, METs calls, or further financial details. Many trauma registries have a number of user defined fields programmed in capturing needed data over the years. So, does ACS recognize this? Absolutely! The very next sentence chapter 15 after CD 15-9 states: “This staffing need increases if additional data elements are collected.”[iv] ACS clearly recognizes that hospital level trauma registries contain so much more data than what is reported to the National Trauma Data Bank (NTDB). They recognize this because they note that “the trauma registry is an important management tool that contains detailed, reliable, and readily accessible information needed to operate a trauma center.”[v] Now that we have explored the FTE requirements, data elements, additional data elements, as well as the need for a “well-trained” trauma registrar, we need to address several other key “productivity” factors. Factor #1, the trauma registry software. Each software vendor is different, therefore each software has its own unique way of laying out its pages, shortcuts, as well as data entry “tricks”. One package may have a minimum data set above and beyond the NTDS, and others may have every possible field you can imagine ready to “collect”. Some software packages use unique ICD-10 to Abbreviated Injury Scale (AIS) mapping, others require you enter each separately. There are no “right” or “wrong” ways, only pointing out there are differences. Factor #2, your hospital Electronic Medical Record (EMR). There are a number of commercial products on the market, from Allscripts, Cerner, EPIC, and McKesson. Each unique, each valuable, but each set up differently. EMR questions to ponder are: how complete are they? Do you need to go to an additional system to retrieve certain pieces of data (EMS, Labs, ED, etc.) or is everything in one place? Are all documents there? One of the biggest missing pieces of documentation in EMRs are the EMS run sheets. If this is missing do you have to go to a state EMS bridge to retrieve them? Contact the EMS agency? How much time is involved in your EMR processes? Factor #3, the experience level of the trauma registrar. If your trauma registrar is a novice, they may not even realize what they do not know at this point. Therefore, data validation and training are key factors. Is the trauma registrar a competent practitioner? They will demonstrate confidence, act as a resource to the novice registrar, and they should have a high inter-rater reliability (IRR) each month. Is the trauma registrar an expert? Are they preforming the data validation, acting as the resource for the team, understanding the data for reports, research, and performance improvement? This is a critical area that you must take into consideration. In practical terms, the expert trauma registrar has most likely memorized key injury and procedure codes, therefore, they can move quickly through a chart. The novice may spend more time in the chart as they are looking up these codes, or potentially even looking up the injury itself before trying to code it. The novice registrar should be focusing on lower acuity charts, while the expert is focusing on the severe or complex charts. Factor #4, chart acuity. As stated in factor #3, experience level is important but also should match up with chart acuity level. The more experienced the trauma registrar, the more complex or higher acuity chart they should be taking. Chart acuity can be measured by factors such as outcome (deaths), ICU admissions, highest level of trauma activation, or by injury severity score (which only comes after the chart is abstracted). Chart acuity is pivotal in comparing trauma registrars. There is just no clear apples to apples comparison. Lastly, reviewing your processes. It is critical to every program to work efficiently. This transcends into every aspect of the trauma registry. For example, review the process for identifying the injured patient. Has your EMR system changed over the last few years? Is there a better report? Can you create a patient list within your EMR which can notify you of a patient’s discharge? These are all ways to streamline processes. The critical point is to review the data elements that you collect. This is recommended to be reviewed at least twice a year. Do you still need all of this data? If so, is it required on all patient, or a subset of patients? Is the data element (work) redundant? For example, entering in the results of an X-ray or CT scan can be viewed as redundant. If the X-ray or CT scan had a positive result, there would be a corresponding injury in the AIS / ICD-10 injury list. Another item to ponder is how many times are you in the EMR / trauma registry record for a single patient? How can you possible streamline this process? Does every open patient require daily updates, or a certain subset of patients (such as ICU admissions)? Sometimes this step requires you to think outside the box so to speak. Looking for new ways to do the work is intimidating but can be rewarding. For example, an EMR download into your trauma registry to fill in fields such as date of birth, address, insurance, or even ED arrival time. If the EMR is not capable of this, can you establish a “trauma registrar” pathway where the data screens, flowsheets, and information are all grouped together? This would cut down on the time spent searching in the EMR, or at least streamline the process by grouping the data needed. As you think outside the box, also think about the experience level discussed in Factor #3. The new hire or novice should get all of the 1-day length of stay patients. While they may get the “lions share” of charts, these are minor injuries and are a good training ground for the novice. Likewise, the expert registrar would take the complex charts. It will take them much longer to abstract the chart due to the acuity, but it will be accurate. Now how do you put all of these factors into a productivity formula and get meaningful data? The Buck Data Validation System (BDVS) is a comprehensive system that helps with just this situation. When used for data validation, the end reports allow the manager to: simultaneously track trauma registrar productivity as well as their individual IRR scores. This system cuts data validation time in half and allows you to focus educational resources exactly where they are needed. So how does this all work? The trauma registrar enters into the BDVS system the trauma registry number, the date and time the chart was started, the date and time it was completed. Additionally, they enter in the trauma registry ISS, ICU and the hospital length of stay (LOS). From these minimal data elements, the BDVS system can generate the total time spent abstracting the chart, as well as charts that should be targeted for data validation. Data validation is performed by a second abstractor and results are entered into the BDVS system. The IRR is automatically calculated per data element, per chart, and per abstractor. Additionally, the project manager will have a report that demonstrates the total team outcomes, as well as the individual team member. As you can see, Trauma registrar #1 averages 1 hour and 25 minutes per chart and has an average ISS of 12. Their average ICU LOS is 2.33, and average hospital LOS is 6.33. Most importantly, their IRR is 94.34%, with 100% accuracy on injury coding, 95.65% on procedure coding, and 100% on Pre-existing conditions (which is important in risk adjusted benchmarking). Now let us compare that to registrar #3, Their average chart abstraction time was 47 minutes, with an average ISS of 16. (So far registrar #3 looks great!) Their average ICU LOS is 0.5 days, and hospital LOS average is 6.5 days. (their patients were not in the ICU very long) Their IRR is 91.5% with 96.4 % accuracy in injury coding, 96.97% in procedure coding, and 100% in Pre-existing conditions. In this comparison, registrar #1 took longer per chart, but also had a higher IRR. Registrar #3 was faster, but accuracy was a factor. This is great meaningful data. This is specific to your facility, your processes, and your staff. The BDVS give a team summary for productivity and accuracy as well. This is information that every trauma registry lead, and trauma program manager should have on their team. This is information that will help answer the questions about productivity, and balance that with accuracy. In this example we see the average time in the chart is 1 hour and 7 minutes, but the overall IRR is only 88.7%, with injury coding being 91.7% accurate, and the Pre-existing conditions only 66.7% accurate. This translates into, a “higher” productivity rate, but less accuracy. In this example the Pre-existing conditions were 33.3% of the time wrong (66.7% accurate). This is the data that will drive your risk adjusted benchmarking reports, as well as determining your facility’s placement when compared to like centers. Are you a under-performer? Or is your data an under-performer? The BDVS system also has visual graphic outputs for data visualization. Can you spot patterns within your team? Are there ups and downs with productivity? Is this type of data visualization a team motivator? As you still ponder the age-old question of productivity, and accuracy, consider speed verses accuracy tradeoff. This is a complex relationship. Do you want a trauma registrar to respond slowly, making relatively fewer errors, compared to a registrar responding quickly, rushing through a chart, and thus making more errors? Heidi Grant-Halvorson said it best, “human thought, like every other complex process, is subject to speed-verses-accuracy trade-off. Go fast, and you make mistakes. Be thorough and diligent, and you take an eternity. We are motivated tacticians – strategically choosing ease and speed, or effort and accuracy, depending on our motivation.” What will be your motivation for your team? Accuracy or Speed? First establish a baseline and know where exactly you are starting. Monitor for several weeks, then analyze the data. At that pivotal point, choose your motivation, stress its importance, and continue to monitor. There is no easy answer, only hard work, diligence, and transparency, as “TRAUMA” is a team effort! [i] American College of Surgeon: Resources for Optimal Care of the Injured Patient: 2014, Chapter 15, page 112
[ii] National Trauma Data Standard Data Dictionary: 2021 Admissions, page IV [iii] National Trauma Data Standard Data Dictionary: 2021 Admissions, Table of Contents [iv] American College of Surgeon: Resources for Optimal Care of the Injured Patient: 2014, Chapter 15, page 112 [v] American College of Surgeon: Resources for Optimal Care of the Injured Patient: 2014, Chapter 15, page 107 Comments are closed.
|
Archives
June 2021
Categories
All
|
Comprehensive Trauma Program
CONTACT |
|

 RSS Feed
RSS Feed